Understanding the hemorrhoids pathophysiology, causes, sign and symptoms, work up treatment and management
- Be Healthy
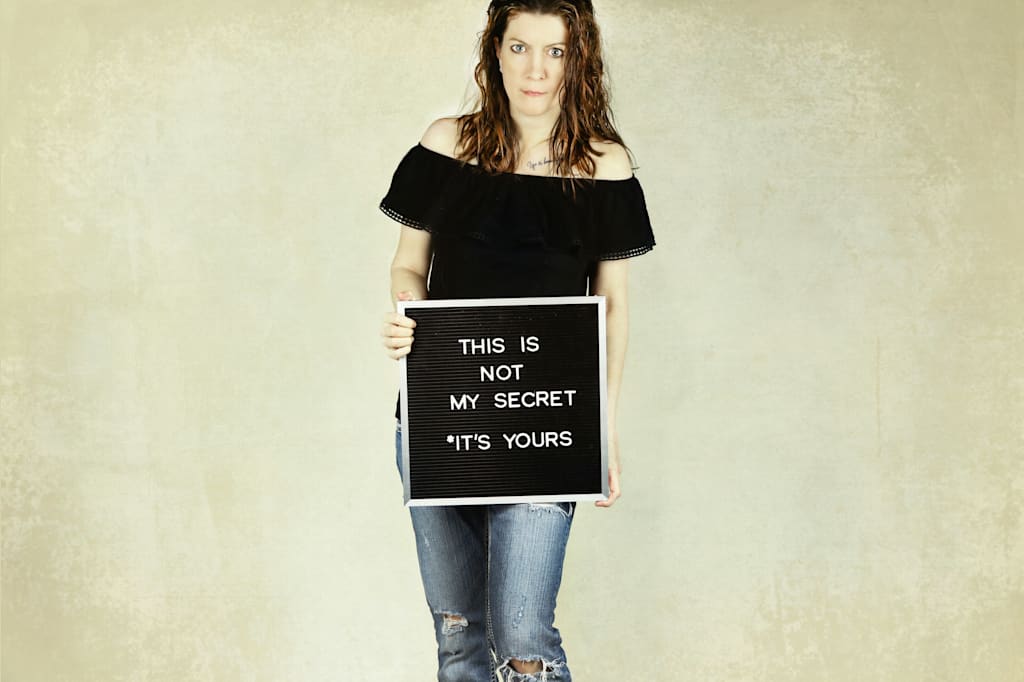
What are hemorrhoids?
Hemorrhoids is engorgement of the venous plexus in the anal canal. The best way to start is going to be with the anatomy of the anal canal.
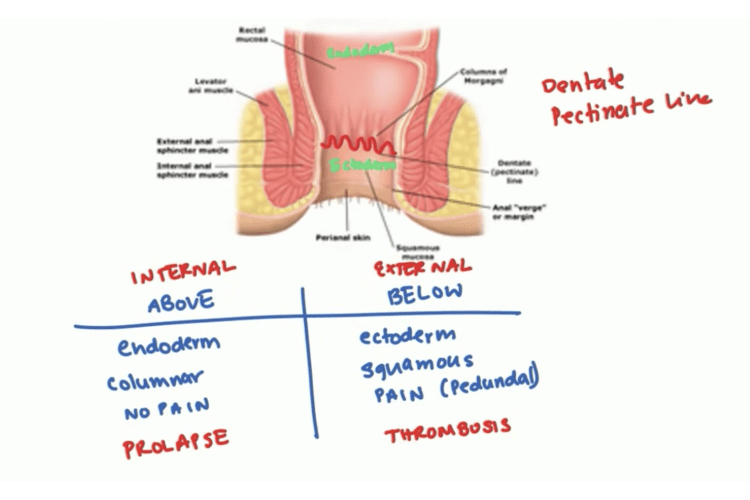
The anal canal so we now have a diagram here of the inner canal. The most important part on the anal canal is going to be this line that I havedrawn here. That’s called the dentate or also known as the pectinate line. This is really really important because early on in embryology there this is a combination of two different embryological parts.
Above the pectinate line, you have the endoderm and below the pectinate line you have the ectoderm. Let’s draw a table then we are right above for above the pectinate line and below for below the pectinate line line.
We will compare and contrast are the different features.
Above is going to be derived from the endoderm of the embryological tissue and below is going to be derived from the ectoderm of the embryological tissue. This also means that the type of cells are going to be different.
In the endoderm you have the columnar cells and in but below the pectinate line you have the squamous cells. Just as a side note this also is links into pathology related to cancer.
So generally above the pectinate line you get adenocarcinoma and below the packing line you get squamous carcinomas and this is just because of the histology.
Since the above the packing line is there for the endoderm there isn’t no necessarily somatic sensation so there is no pain above the pectinate line. However below the pectinate line this is going to be pretty much your skin and your skin has somatic sensation and this is going to be you will feel pain.
Primarily the nerve that this sense the sense goes through is the pedundal nerve. So the pedundal nerve is a nerve involved in feeling this pain.
When it comes to pathology that we are going to talk about today with hemorrhoids it is I guess one key feature is hemorrhoids that are above the pectinate line off sometimes result in prolapse whereas hemorrhoid below the pectinate line result in thrombosis.
Since we are already kind of jumped the gun here hemorrhoids above the pectinate line are also known as internal hemorrhoids and below the packet line are called external hemorrhoids.
Etiology: the causes of hemorrhoids
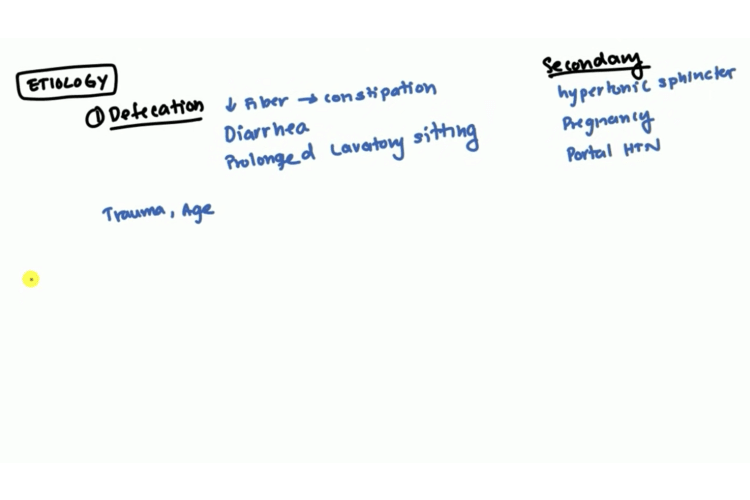
Defecation is the primary cause of hemorrhoids
The first etiology is going to be related to defecation because that’s the primary you know function of the anal canal. So generally patients who have low fiber diets what will happen is because they don’t have enough fiber the diet they tend to become constipated and when the patient becomes constipated they strain very heavily and this can be to increase abdominal pressure and it can engorge the via the veins of the anal canal and we will talk about those very specifically in a little bit.
Also constant diarrhea can agitate the size of the walls of the anal canal and that can lead to this type of the veins. And also believe it or not prolonged laboratory sitting. These are generally people who when they use a toilet they end up reading a book for hours or whatever. This can block the flow around the anal canal and this is one of the cause for hemorrhoids. If youare one of those people might want to read your book on the sofa instead.
Also trauma can lead to it and even age as you get older some of the support structures tend to weaken up.
Besides defecation there are there are some secondary causes so other pathologies that can lead to hemorrhoids.
Hypertonic sphincter : a secondary cause of hemorrhoids
The first first is going to be a hypertonic sphincter. When patient has a - hypertonic sphincter it makes them push harder while they are defecating. And then this is can cause increased abdominal pressure which can lead to engorgement up those anal vessels.
Pregnacy is another secondary cause of hemorrhoids
Pregnancy can also lead to it and again pregnancy a lot of times is caused increased abdominal pressure and that is a little cause. Of course portal 2 hypertension you know oftentimes caused by liver cirrhosis.
Hypertension can lead to hemorroids
And then of course we know for hypertension it could also cause esophageal varices anal varices and even the umbilical varices.
That is just your general causes now we can go back into different types of hemorrhoids.
Different types of hemorroids
We are talking about types I have kind of already alluded to it earlier.
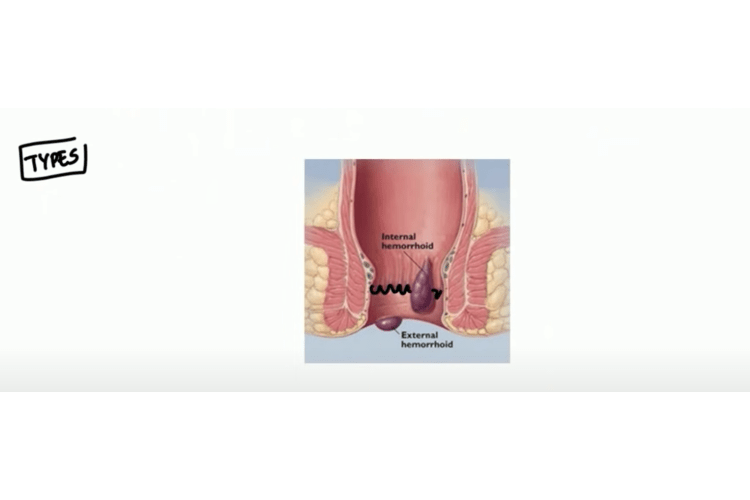 As you can see here is a pectinate line. Hemorrhoids that are above the pectinate line such as this one are going to be internal hemorrhoids and hemorrhoids below here and outside the anal canal is going to be your external hemorrhoid.
As you can see here is a pectinate line. Hemorrhoids that are above the pectinate line such as this one are going to be internal hemorrhoids and hemorrhoids below here and outside the anal canal is going to be your external hemorrhoid.
That is how they are divided.
So we know the veins are involved so it’s important to go over which actual veins we have in the canal. The first in the internal area we have something called anal cushions and in the external we have we just have circumferential veins.
So you you know right here kind of drawn a diagram of the actual blood supply of the internal and external canal.
The internal and external hemorrhoids
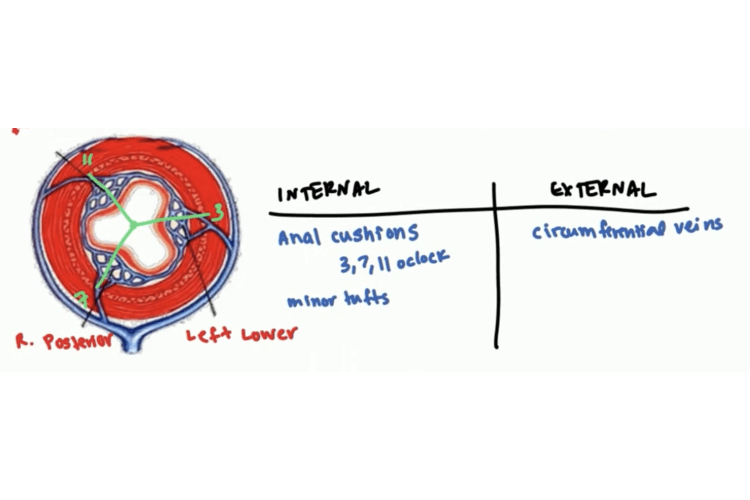 So what you can see is you can see this plexus is 1 2 and 3. These 3 plexuses are the anal cushions that are found here the internal canal. Out here and the external here this is the circumferential vein. This is the major sight of pathology when we start talking about hemorrhoids.
So what you can see is you can see this plexus is 1 2 and 3. These 3 plexuses are the anal cushions that are found here the internal canal. Out here and the external here this is the circumferential vein. This is the major sight of pathology when we start talking about hemorrhoids.
The one right here is called the left lower plexus of veins or the left lower anal cushion. The one down here is called the right posterior anal cushion and the one on the top is called the right anterior anal cushion. So right away says this is enter your you know your genitalia is on this side this is kind of your backside there.
These are your three plexuses that counting it aboard and so since this is the main locations generally what you have is you have hemorrhoids you get second. So what I have drawn in green here is if you think of this as a clock this being twelve o’clock you generally get one hemorrhoid at the three o’clock position you’ll get one the hemorrhoid at the seven o’clock position and 11 o’clock position.
Mixed hemorrhoids
Mixed hemorrhoids is basically when you have a hemorrhoid that starts off an internal cross the pectinate goes at the external so if it goes into both that’s called a mixed hemorrhoid.
Grades of internal hemorrhoids
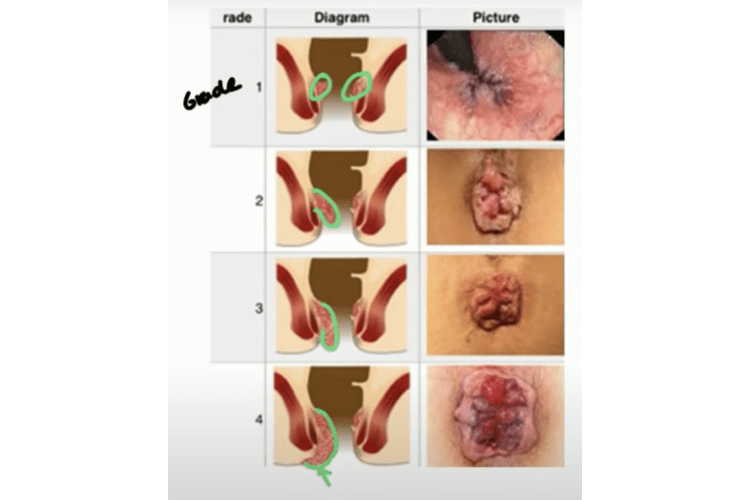
Internal hemorrhoid sensitive prolapse they have different grades based upon how much they prolapse.
Grade 1 of internal hemorrhoids
The first one here is grade 1. In grade one there is no pull up so you can see there’s like just these two little like nuggets there. So there is no real prolapse and then on the right hand side we have a picture there and you can see when you visit we look at the anus there’s really nothing there to see from the outside in.
Grade 2 of internal hemorrhoids
You can see that the hemorrhoid is bulging out so kind of highlighted in green.
However its bulging out and and generally what happens when they defecate it will come down and it will spontaneously regress.
So you have spontaneous regression is a key feature of grade 2. You can see here that the grade 2 is you can actually kind of see it visibly.
Grade 3 of internal hemorrhoids
I have kind of highlighted it there in grade 3, whenever they defecate the prolapse will increase.
However what digitally they can push it back in and so you can see here it’s you know it’s protruding much more than great. So digitally they can pull back to grade 3.
Grade 4 of internal hemorrhoids
The final most severe grade is great forward so you can see the whole thing bulging there and you know in grade four that the distribution did the distinguishing feature between Grade three where four is if you apply pressure up this way it won’t reduce it’ll just stay up.
So grade three you could manually regress it however in grade four it’s no way to regress it so and you can see how big that and you can just see as you go as you go down it’s become bigger and bigger and more visible so that’s internal.
Grades of external hemorrhoids
We know that external is a circumferential vein and so they can occur anywhere they don’t have the same three seven eleven o’clock thing. The biggest problem with external is trombosis.
Here’s an image here of an external hemorrhoid and you can see the kind of blue discoloration. That is troubles right there so you can see that and what I happens oftentimes is it begins to erode the skin and that can eventually lead to bleeding bright red blood so that’s a common feature of external hemorrhoids.
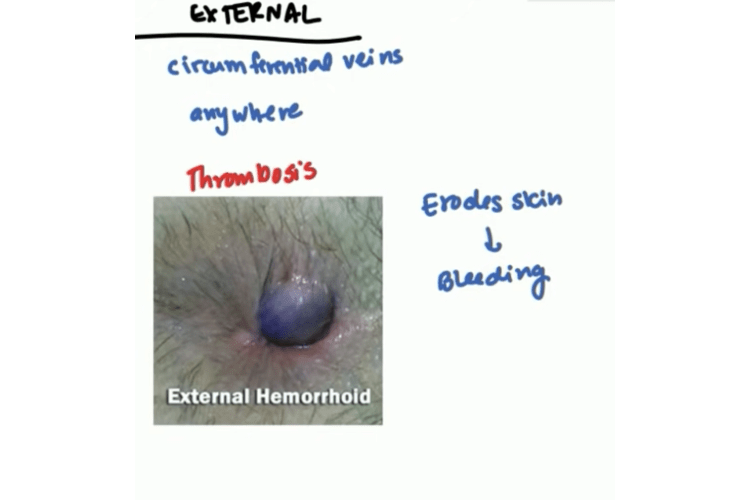
Chronic external hemorrhoids
When it becomes chronic they can actually produce skin tags. You can see skin tags here and the problem with skin tags is there’s many crevices. So you have like one here there you know we have like three four too long on there and so what I can happen is a hygiene becomes an issue.
When they defecate the fecal matter it gets trapped in this area that can lead to intense itching and of course infections as well later.

As you can see, external hemorrhoids is not as bad as internal hemorrhoids because it’s does have that prolapse and the prolapsed can lead to different complications. Let’s talk about that.
Hemorrhoids complications
When you have a prolapse, what can happen is often times you can get the external sphincter can compress it and so when the external sphincter compresses it you get decreased venous return and that leads to strangulation. Once you have strangulation of the actual prolapsed piece I guess you can say this can either lead to fibrosis of that piece or gangrene of that piece.
Of course you have gangrene that’s going to be much more seriously to surgery in here fibrosis.
I guess it’s not as serious but once you have strangulation what can also occur is you can have that piece ulcerate or it can thrombosis.
If it trombose that can lead to pain and if it ulcerate that can lead to bleeding. This is the common symptoms of hemorrhoid is pain and bleeding.
So generally that’s going to be your complication related to prolapse, especialy if it has been there for a long time meaning it’s trapped into the sphincter.

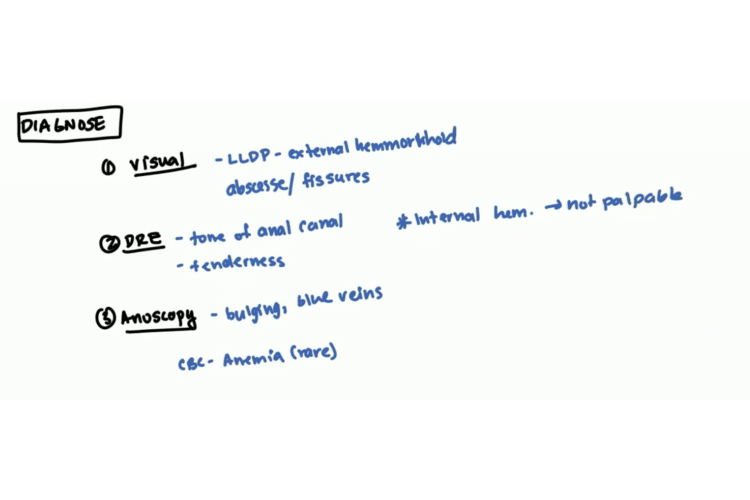
How do we diagnose hemorrhoids
First of all you are going to want to do a visual inspection. You do a visual inspection up foot by first putting the patient a lateral left to keep this position. Generally to have an external hemorroids you can see it right away.
However while you are over there you do want to try to rule out abscesses and fissures. This is because many patients will come in saying I have a hemorrhoid but it’s not a hemorrhoid it’s just just a common condition that they know of they might just have a figure or an abscess.
After the visual inspection is done you want to proceed to a digital rectal exam. In digital rectal exam the first thing we will check is for the tone of the anal canal and you also want to look for any tenderness.
What do you do want to remember that internal hemorrhoids oftentimes are not palpable. Just because you can’t palpate something doesn’t mean you can rule out hemorrhoids and so obviously if that’s the case that we are going to have to do also do an anoscopy.
What you generally will find is like a bulging blue veins and so if you see that you pretty much diagnose internal hemorrhoids at that point. There’s no really need to do any more investigations labs imaging. Sometimes this has been chronic or it’s really bloody you can do CDC to let anemia but that’s very very rare so not commonly done.
Hemorrhoid treatments
Once you diagnose it of course we want to go into treatment. Let’s talk about that.
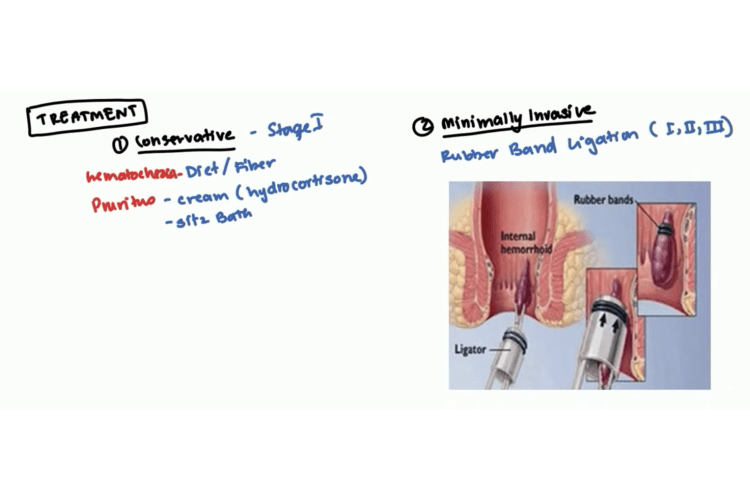
Conservative treatments
The first line of treatment is going to be conservative treatment and you are going to want to do that whenever it’s stage one not the stage wanted to say that whenever you have a stage one you definitely want to start off with conservative.
Maybe you need stage two you want to start off with conservative. The first step is going to be diet and fiber. So as soon as you can change their diet you know maybe give some fiber supplements, get exercise that can help some of the symptoms a lot and actually it has been shown to actually decrease the hematochezia that they might have. Hematochezia just means blood and the feces.
With regard to pruritus which does occur sometimes, oftentimes you can give cream hydrocortisone. It’s very common and sitz bath is also helpful for them you know to kind of alleviate some of the symptoms is going on.
Minimally invasive treatments
Once you try to conservative treatments and you know say doesn’t work then you do need to go to minimally invasive treatment.
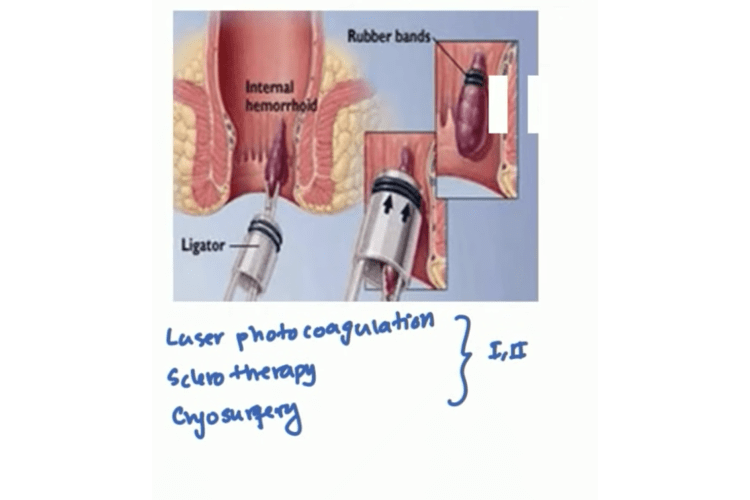
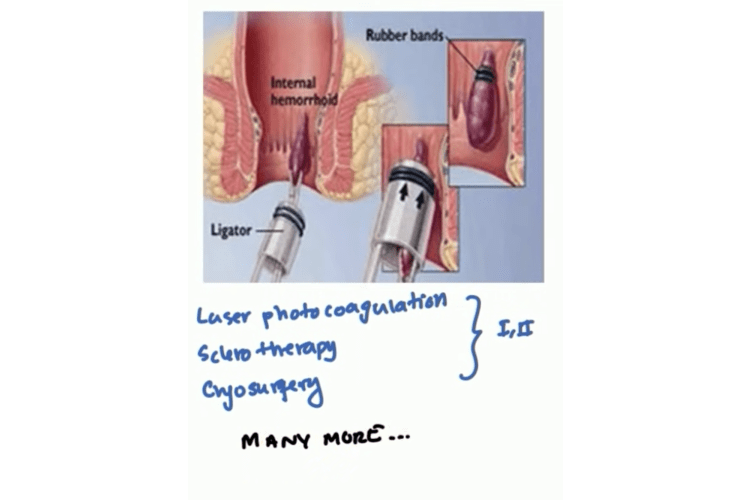
Minimally invasive is basically any type of procedure that can be done in the OPD clinic so the outpatient clinic that you can do it there. The most common one most popular is the rubber band ligation.
The rubber ligation can work for stage 1 2 or 3 however it doesn’t work for 4. What would you do in rubber band ligation so here here I have a diagram of what happens.
You have this device here called alligator. If you clamp the hemorrhoid and then you push the ligator up above the hammer to suck it in and you see use this black area here. These are rubber bands you take them off and these rubber bands will clamp the hemorrhoid shut. So after a while it stops the blood flow and it just will come right off. It is very quick non-invasive painless way to treat the condition. This is the most popular way to do it.
However there are other options for the reasons you know that needs to be done.
One of them being laser photocoagulation which is they use high intensity light beams, sclerotherapy where they sclerose the actual hemorrhoid and finally you have cryosurgery where they make it really really cold.
So you can use this those three on stage one and stage two not stage three or four.
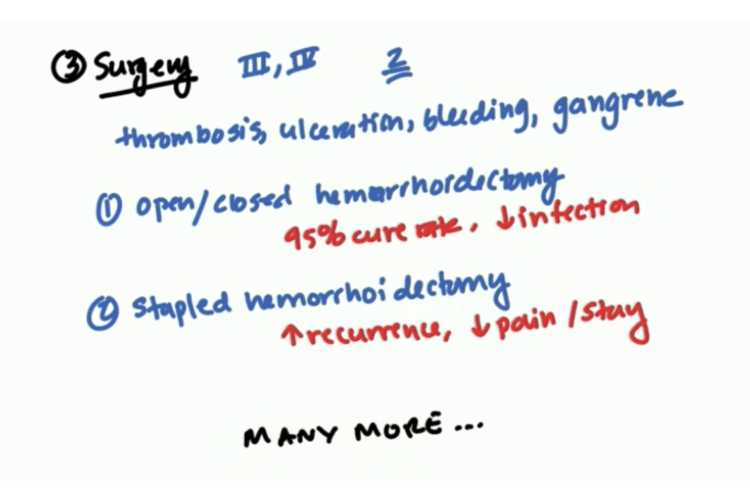
Surgery
Surgery is generally reserved for cases where it’s stage 3 or stage 4 and sometimes 2, if the conservative management and minimally invasive management didn’t work. You also want to do this if they have thrombosis. You want to do this if there’s also ulceration, if you find any bleeding or if there’s gangrene.
Open or closed hemorrhoidectomy
So any of those four conditions can automatic surgery. The common surgeries that are done is known as hemorrhoidectomy. You can have an open or closed hemorrhoidectomy.
These are these were pretty effective. They have about a 95% cure rate and infection rates really really low.
Stapled hemorrhoidectomy
There is another method which is called the stapled hemorrhoidectomy. This has a higher recurrence rate however there’s less pain and it’s a shorter stay so some patients prefer this.
Now with regards to hemorrhoids is a very common condition and since it’s very common there’s many different devices procedures being developed. There’s definitely many more I couldn’t get into all of them and that goes with minimally invasive as well there’s definitely many more going on.